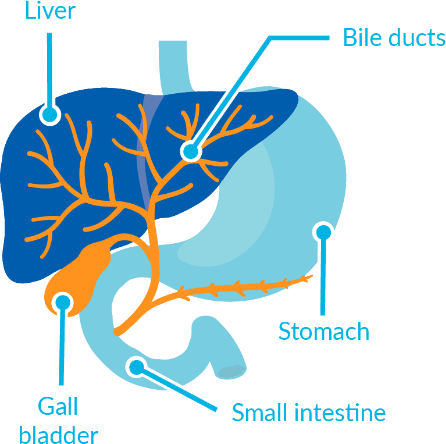
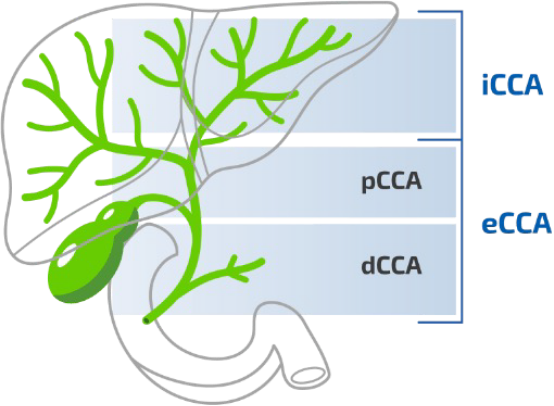
- Cholangio = bile duct
- Carcinoma = a form of cancer
CCA is a rare cancer.2,3 The number of people diagnosed with CCA varies between countries.2-4 In most countries, fewer than 6 in 100,000 people each year will be diagnosed with CCA2,3,5
The lowest rates have been reported in Europe, Australia and the US, and the highest rates in Southeast Asia2,5,6
CCA has become more common in most countries worldwide, including those in Western Europe, during the last 20–30 years4-6



CCA is most often diagnosed in people over the age of 50 years (>65 years in Western countries).2,5 It is slightly more common (approximately 1.5 times) in men than in women4,9
There are many other risk factors for CCA. Some of these risk factors are more established than others2
Some risk factors are common and others are rare, depending on the type of CCA and region of the world2,3,5,6,8-12
Some of the risk factors, such as smoking or being overweight, are not unique to CCA